In the United States, several measures have been developed in order to encourage hospitals to address noise and speech privacy issues. One of the most influential initiatives is the Value-Based Purchasing Program enacted by the Centers for Medicare and Medicaid Services.
This program is rooted in a Total Performance Score for each hospital, 70 percent of which is based on clinical quality assessments and 30 percent on patient satisfaction scores. Hospitals that perform poorly are financially penalized through Medicare withholding, while those that do better are rewarded.
The satisfaction scores are derived from the results of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which is given to a random sample of patients between 48 hours and 6 weeks after discharge. It includes 18 questions, grouped under eight topics. A hospital earns points for achieving a certain level of performance relative to other hospitals, for improving its performance over previous periods, and for consistency across all eight areas.
Since 2007, the quietness of patients’ rooms at night has been the lowest-rated satisfaction marker nationwide, placing noise control at the top of many facilities’ list of objectives. Noise not only drags down a hospital’s consistency scores and patients’ overall rating of their stay, it can also affect market competitiveness because the public can review HCAHPS results online.
Noise and patient recovery
The HCAHPS survey likely focuses on quietness at night because sleep is such an important restorative process, and one that is often disturbed by noise. In fact, researchers have found that the sick and the elderly are the most likely to have their sleep disrupted by noise, and that people never completely habituate themselves to night-time sounds.
Noise reduces both the quantity and quality of sleep, weakening the immune system and impeding the body's ability to generate new cells. A growing body of medical studies shows that it also causes problems during the day. In fact, side effects such as elevated blood pressure, quickened heart rate and increased metabolism have led some researchers to conclude that noise may slow recovery rates, lengthening hospital stays.
Additionally, patients are not the only ones affected. Given that noise can impact caregivers’ concentration, stress levels and fatigue, both the American Hospital Association and the Institute for Safe Medical Practices recommend that medical error prevention programs take acoustics into consideration.
Health insurance portability and accountability act
Speech privacy is yet another acoustic concern in hospitals. Introduced in 1996 by the U.S. Department of Health and Human Services, the Health Insurance Portability and Accountability Act (HIPAA) requires healthcare entities and other organizations that work with Protected Health Information to take “reasonable safeguards” to ensure privacy during in-person and telephone conversations with patients and between employees.
Though HHS has elected to address speech privacy issues on a complaint basis and few monetary penalties have been issued to date, a hospital must be able to demonstrate that it has investigated acoustics, researched possible solutions and implemented economically viable ones.
The ABCs of acoustics
If one focuses on the types of noise created by building occupants and small medical equipment, there are three key ways to improve noise control and speech privacy in hospitals: absorbing, blocking and covering.
The best opportunity for absorbing noise is typically presented by the ceiling; therefore, installing a good tile and ensuring consistent coverage throughout the building is vital. Hanging absorptive wall panels on large vertical surfaces and key reflective locations (e.g. corridors) may also be needed. Soft flooring can be used to lessen footfall and other ‘traffic’ noise as long as it is implemented in a manner that does not compromise sanitation or hamper the movement of patients and equipment.
Constructing private rooms is the most common method of blocking noise. However, a well-planned layout can also be used to minimize its transmission. For example, high activity areas should be located in areas that are well-separated from patient rooms, and doors facing each other across hallways should be offset. It is also helpful to rethink traditional aspects of the hospital landscape. For instance, nursing stations can be decentralized in order to prevent large groups from talking near patient rooms.
Covering noise is accomplished by installing a sound masking system. This technology basically consists of a series of loudspeakers integrated in a grid-like pattern above the ceiling, as well as a method of controlling their zoning and output. The loudspeakers distribute a comfortable sound that is similar to softly blowing air.
Though adding more sound to the facility seems to contradict the goal of controlling noise, an effective acoustic environment relies on the provision of an appropriate noise floor or level of continuous background sound. The masking sound covers up noises that are lower in volume and diminishes the impact of those that are higher by reducing the magnitude of change between baseline and peak volumes in the space.
For this reason, sound masking has also been found to be a very effective method of improving sleep (Stachina et al, 2005). Similarly, sound masking greatly improves speech privacy because conversations are either entirely covered or their intelligibility is reduced. However, because it requires some distance to become effective, masking does not prevent staff and patients from communicating with one another.
In order to achieve a consistent level of effectiveness in the often highly fragmented environment of a hospital, the sound masking system must be designed to offer small adjustment (i.e. volume and frequency) zones of one to three loudspeakers throughout the facility. Networked control from a location below the ceiling (e.g. from a control panel or software) is also key because opening the ceiling has the potential to spread contaminants into the occupied space below. Also, as described in the 2014 FGI Guidelines for Hospitals and Outpatient Facilities, patients and staff should be able to adjust the masking volume according to individual needs. In this way, the system will not only improve comfort, but also increase patients’ sense of control over their environment, raising satisfaction levels and HCAHPS scores.
Reducing noise through policy
While the majority of the acoustical burden must be borne by the facility’s design, efforts to control noise and protect privacy should not stop there.
The hospital should also designate a person who will document speech privacy practices (as required by HIPAA), provide privacy awareness training for employees, and act as the contact for complaints. In addition, a committee should be appointed to develop, publicize and enforce behavioral policies related to noise. Lastly, administrators should continue reduce or eliminate unnecessary noise sources wherever possible (e.g. fix or replace faulty equipment, such as squeaky carts).
However, in the end, people will always create noise in a busy, round-the-clock healthcare facility. By considering acoustics during the planning and construction of hospitals, one can help meet regulatory requirements, relieve some of the environmental stress from caregivers, and create more comfortable places in which patients can rest and recuperate.
Niklas Moeller is the vice-president of K.R. Moeller Associates Ltd.

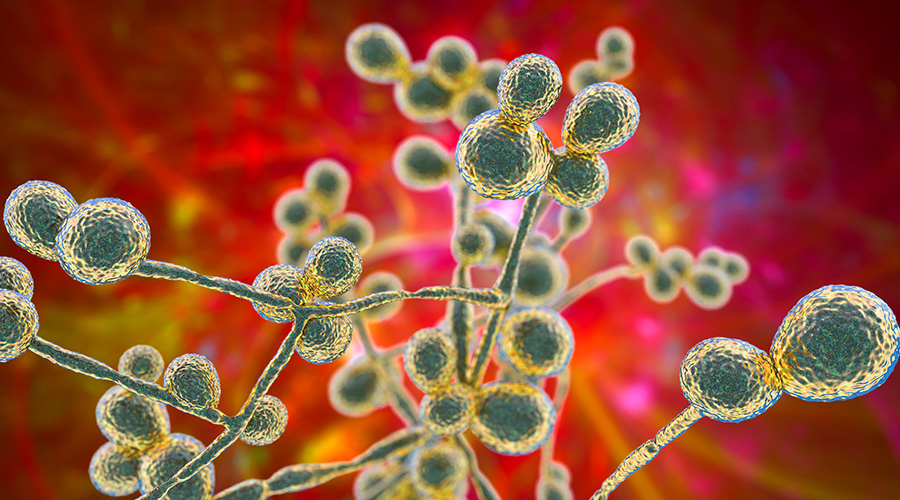 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments