The first months of the COVID-19 pandemic caused healthcare facilities to disinfect surfaces at greater frequencies than people and surfaces could stand. As it became clear that surfaces played a minuscule role in transmitting the coronavirus, greater questions arose regarding the trade-offs associated with the increased cleaning and disinfection efforts.
Healthcare facility leaders questioned if the efforts were worth it. They saw the chemicals caused irreversible damage to equipment, furniture, furnishings, finishes, electronics and other surfaces.
More importantly, was the inordinate spraying of U.S. Environmental Protection Agency’s List N disinfectants exposing environmental services workers, staff and patients to asthma-related health complaints? Years of research have proved the impact of certain chemicals that cause chronic respiratory conditions in those in the custodial job category.
An environmental microbiome exists that is disrupted every time a surface is cleaned. As with the human biome when patients suffer overgrowth of Clostridium difficile (C. diff) following antibiotic therapy, exposure to many disinfectants removes resident flora on environmental surfaces, leaving a vast area of space available for other microbes to contaminate.
In January 2015, the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health (NIOSH) was notified through its Health Hazard Evaluation program of eye, respiratory and skin problems among environmental services staff thought to be related to disinfectant use in a hospital.
In 2014, the hospital had introduced a new disinfectant product with active ingredients that included hydrogen peroxide, peracetic acid and acetic acid to mitigate healthcare associated infections (HAI). The study showed this disinfectant product was associated with mucous membrane and respiratory health effects.
Risks of mucous membrane irritation and asthma in healthcare workers should be considered in environmental services protocols to protect patients from HAIs. Hospitals should select the best disinfecting protocols that reduce worker exposures while maintaining patient safety.
The standard for every healthcare institution is, first, do no harm. There is no need for compromise in choosing the right disinfectant for a facility. It is not a binary choice between killing C. diff and C. auris while protecting the health and safety of patients and staff.
Managers selecting the best disinfectant should consider the following:
- Kill claims for the most prevalent healthcare pathogens transmitted by contact with skin or gloves should be a high priority.
- Fast kill times of less than five minutes. Fast kill times are important because they provide confidence that they are killing the prevalent and most common healthcare-associated pathogens before the disinfection solution can dry.
- Safety reflected in the Hazardous Materials Identification System (HMIS) score. Chemicals should have an HMIS rating of 1-0-0 — slight health risk — or 0-0-0 — minimal health risk.
Ease of use is another consideration to use in evaluating before choosing a disinfectant. Products should be effective in the presence of environmental factors, such as organic matter — i.e., blood — have an acceptable odor profile, be stable, be soluble in water, have simple directions for use and have good cleaning properties.
J. Darrel Hicks, BA, MESRE, CHESP, Certificate of Mastery in Infection Prevention, is the past president of the Healthcare Surfaces Institute. Hicks is nationally recognized as a subject matter expert in infection prevention and control as it relates to cleaning. He is the owner and principal of Safe, Clean and Disinfected. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. He can be reached at darrel@darrelhicks.com, or learn more at www.darrelhicks.com.

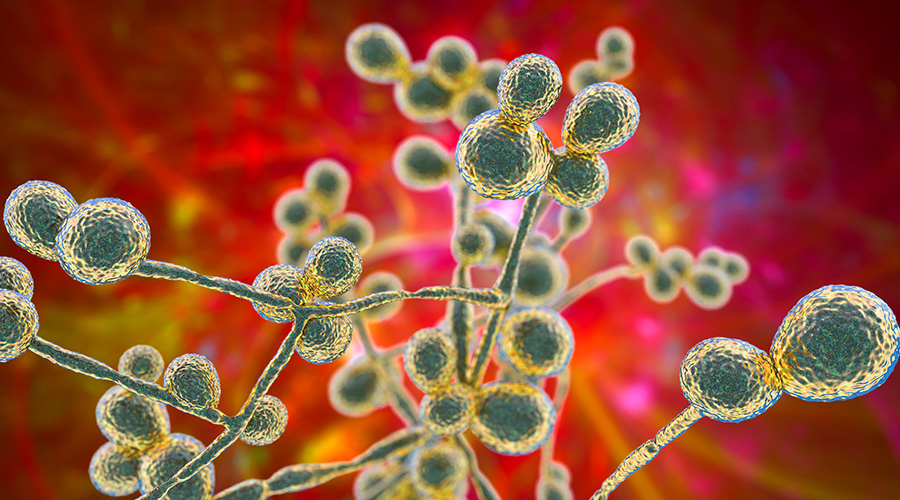 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments