As the Democratic Republic of Congo is currently mired in a health emergency, working to contain an outbreak of the deadly, highly contagious Ebola virus, all nations look inward and ask: are we prepared?
Concerns crescendo about Ebola’s global reach with this new crisis, we vividly recall its frightening, first-time U.S. arrival in HKS’ headquarter city in October 2014, at Texas Health Presbyterian Hospital Dallas – a facility we designed and have been proud to continue working with for more than 50 years.
It was a difficult and stressful time for the hospital, its staff, patients, and the entire Dallas community. As a leading planner and designer of medical and healing facilities, the Ebola crisis in our own backyard presented an opportunity to critically reconsider infection control in our health client’s operations: the flow of staff, patients and visitors through the space, the donning and doffing of personal protection equipment – including secondary people watching – minimizing disruption of care and more.
Back in the 1980s, anterooms were thought to provide a safety zone in which putting on personal protection equipment (PPE), handwashing and de-gowning could be properly executed. It also presumed additional protection by not allowing air from the room of the infectious patient to mix with the air of the “clean” zones of the hospital. Over time, these rooms were considered unnecessary as negative pressure in the room could prevent air from escaping, and hand-cleansing stations could be placed anywhere.
Enter Ebola. When the crisis first arose in 1976 in central Africa, infectious disease experts did not know how the virus was spread. Understanding how infectious pathogens propagate is critical to preventing deadly outbreaks. Once experts discovered that Ebola is transmitted through direct contact with infected bodily fluids versus airborne, the global medical community understood how to control transmission – and health facility design plays a part.
Ebola claims its victims quickly, and often — left untreated, people contracting Ebola usually die within a week, and the disease is fatal in 50-90% of cases. The highly viral and lethal nature of the disease caused hospitals to reconsider their infection control strategies, and possibly reintroduce the anteroom.
In a thorough review of the clinical process, workflows and infectious disease safety principles, we found there is not a need for a separate compartment prior to entering a room where a highly infectious patient is being treated.
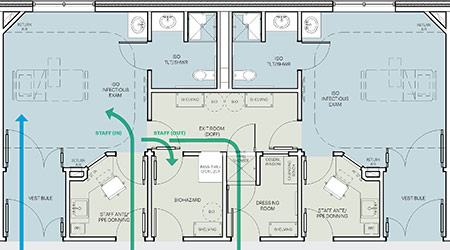
The problem resides with the room exit. All the PPE, once used, is assumed contaminated. Further, when someone exits a room rapidly, air currents created through physical body movements can overcome the negative pressure pulling air back into the isolation room. In fact, this violates one critical general principle of contamination handling: never backtrack. Our exit room concept eliminates dangerous backtracking of contamination within a medical facility.
Some key exit room features include:
Unidirectional flow of the caregiver. The flaw of the anteroom concept is that contaminated individuals return the same way they came in, potentially infecting the clean area of the unit. Like a drive-through car wash, the concept leverages unidirectional flow throughout various stations, with the caregiver never returning the same way they came in.
Sufficient gowning space. As an enclosed anteroom adds considerable cost and obscures patient visibility, our concept provides efficient space utilization through a gowning “station” providing access to PPE and hand-cleansing near the entry, while still allowing direct visualization of the patient by the clinical staff.
Air filtration & disinfection measures. Self-decontaminating surfaces, overhead or portable UV or HINS lighting for disinfection and dual in-line HEPA-filtration (on exhaust and single on supply) features ensure critical safety systems are in place.
Wash stations, “Shower-out” systems aligning with BMBL Guidelines. The room provides all necessary elements for safe de-gowning, showering, and containment/disposal of all contaminated materials in compliance with Biosafety in Microbiological and Biomedical Laboratories guidelines, a publication of the CDC directing facility design and operations in sound containment and biosafety principles.
Waste containment / Liquid waste collection and treatment. Ebola has taught us that any comprehensive infectious disease isolation strategy must address contamination that can occur from exposure to infectious body fluids. The exit room eliminates backtracking because there is no return option for people or contaminated waste to the clean area. The room configuration allows for either decontamination or containment and proper disposal of contaminated items.
Protocol checklist. Workflow includes a protocol checklist, requiring verification by a second health provider.
With the use of an experimental Ebola vaccine limited to only those who have encountered the virus firsthand, providing strategic ways for health facilities to minimize the exposure risk and the virus spreading is essential. There is no doubt that facility design is just one vital part of an equation that includes operations and comprehensive staff training.
Our innovative exit room concept, created in an interactive design charrette with physicians, clinical nurses, architects and contractors, has been implemented in two medical systems in Texas, and HKS’ health design leaders are looking forward to applying this concept in other projects.
Brian McFarlane, AIA, LSSYB is health group director of business development for HKS. Erin Peavey, EDAC, LEED AP BD, is a HKS design researcher.
 Building Disaster Resilience Through Collaboration
Building Disaster Resilience Through Collaboration Amae Health Expands to New York City
Amae Health Expands to New York City Hospital for Special Surgery Opens Two New Facilities in New Jersey
Hospital for Special Surgery Opens Two New Facilities in New Jersey Should We Be Testing Toilet Water in Patient Restrooms?
Should We Be Testing Toilet Water in Patient Restrooms? Healthcare Union Petitions for Increased Staff Safety at HCA Florida Hospitals
Healthcare Union Petitions for Increased Staff Safety at HCA Florida Hospitals