COVID-19 vaccine-related headlines such as, “Scientists can’t seem to agree” or “Scientists keep changing their mind” have become common these days. But science is always changing. Whether the topic is vaccinations or building codes, the science informing the guidance is a work in progress, a snapshot in time.
The science behind healthcare facilities technology is no different. Failing to evolve hospital building codes with the most up-to-date science can cause facilities to run the risk of added waste, added cost, and added safety risks for patients and staff.
In the case of mechanical systems, hospitals are among the most energy-intensive facilities in the United States, and they are especially large consumers of natural gas and electricity in California. But one California hospital facility director says (the industry at large) been basing air changes per hour (ACH) standards on “legacy numbers” that predate the invention of the electric light bulb, the car, and modern plumbing.
Essentially, many managers in healthcare facilities are over-ventilating spaces, requiring tremendous amounts of unnecessary natural gas for heating and cooling. Specifically, data has shown that hospitals are using 30-40 percent more natural gas than is necessary to meet Indoor air quality (IAQ) standards for safety and occupant comfort, and they have seen little improvement in overall energy efficiency over the last four decades.
Case in point
The California Energy Commission (CEC) issued a grant solicitation in June 2016 to research the larger issue of natural gas efficiency for healthcare facilities, specifically in California hospitals. Mazzetti part of a team that was awarded the grant and partnered with one of the leading healthcare providers and not-for-profit health plans to start the project.
The research team’s premise was that many hospital spaces have high requirements for minimum ventilation rates. Over-ventilation was often suspected in many zones. If ventilation could be reduced while maintaining the standards for IAQ for safety and occupant comfort, the facility would be able to reduce the amount of energy used by the air handling units, chiller plants, and boiler plants.
The team set out to design a system where IAQ sensors installed throughout the facility would trend and analyze real-time air quality data to ensure a safe environment while reducing ventilation rates for each space. Research was conducted to identify an IAQ sensor product that could be cost-effective and non-invasive when installed.
Sensors were installed in 76 locations throughout a four-story, 280,000-square-foot patient tower, as well as one roof sensor to monitor outdoor air conditions. The contaminants that were being monitored included particulates, carbon dioxide, total volatile organic compounds, ozone, temperature, and relative humidity. To the team's knowledge, this is the first time this level of air quality data has been collected for a U.S. hospital.
A conversion from constant air volume to variable air volume (VAV) was performed, which allowed the terminal units to modulate the airflow based on heat load in the space. This was done primarily by reprogramming the terminal units’ supply ventilation setpoints.
Finally, the team implemented a dynamic sequence of operations that enabled those terminal units to further reduce their minimum ventilation rates based on real-time IAQ data readings and predetermined thresholds.
The resulting data indicated no definitive correlation between IAQ and ventilation rates. This means the data set did not follow the theoretical relationship of particles or carbon dioxide increasing with lower ventilation rates. The results also proved that the air quality in a hospital is extremely high compared to that of outside conditions, even at two or fewer ACH.
As a result of the lower ACH rate, the energy savings are significant. Based on the calculated energy baseline, the team predicted: a 50 percent reduction in fan energy, a 36 percent reduction in cooling energy, and a 29 percent reduction in heating energy annually.
The results of the demonstration project influenced a change to the current Title 23, Part 4, California Mechanical Code that previously required modulating flow boxes on the return air side, which has been a barrier to VAV designs. The change removed the return box requirement, significantly reducing the cost for VAV conversion projects.
The project team is drafting code change proposals for ANSI/ASHRAE/ASHE Standard 170-2017, Ventilation of Health Care Facilities, and for California's hospital code, Title 24, Part 4, California Mechanical Code. The proposed changes include lowering minimum ventilation rates for patient rooms and removing positive-pressure requirements for medical prep rooms and clean linen storage, which would allow the ventilation in those spaces to be turned down when demand is lower.
One additional change proposal is being drafted specifically for Title 24, Part 6, CA Energy Code to require VAV in all non-pressure required spaces in a hospital to conserve energy.
Walt Vernon is CEO of Mazzetti, a healthcare design and consulting firm, and founder of Sextant, a not-for-profit committed to developing sustainable infrastructure for health facilities in low-resourced countries. Walt’s 30-plus year career has been dedicated to driving change to help reduce Healthcare’s environmental footprint.
Austin Barolin is senior energy analyst and mechanical engineer with Mazzetti. His expertise includes energy audits and facility condition assessments, identifying the energy conservation opportunities, and developing energy savings calculations.

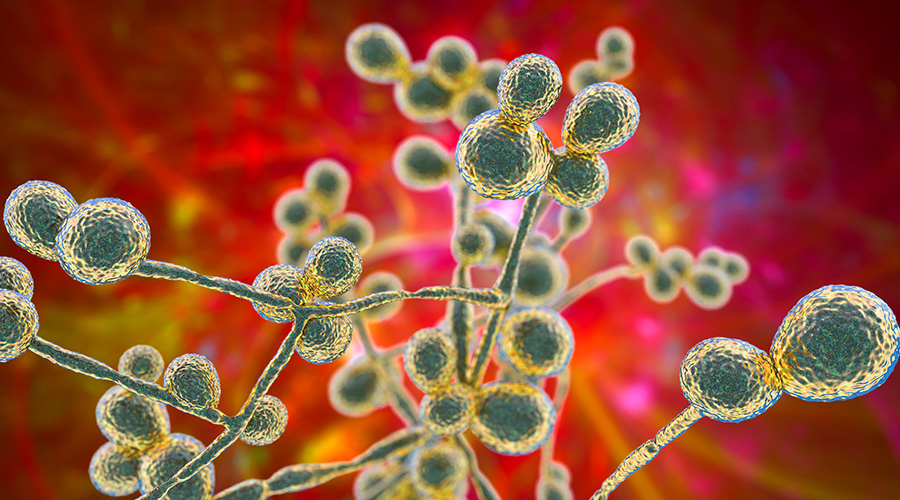 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments