Before Zoom, I was doing an in-person job interview at a prestigious children's hospital in the Midwest. I was interviewing for the director’s position in the environmental services department. Next up in the round-robin schedule for me was sitting with the director of the infection control department, an infectious disease doctor.
She gave me a 10,000-foot view of her role in the hospital and asked me about my experiences with cleaning and disinfection. Then she asked me how I would ensure that a terminally cleaned patient’s room is ready for the little girl who has been waiting for admission from the emergency department.
I thought this was a great time to say that we as a profession need evidence-based objective measurements of surface hygiene by using various methods. Some are using wet or dry chemical markers that are invisible to the naked eye but show up with ultraviolet (UV) light. These markers are removed easily with normal cleaning.
The transparent marker soils are placed on touchpoints before the cleaning is performed. After cleaning, they are checked with a UV light to validate that they have been removed along with any contaminants.
Others seeking evidence are using handheld meters that test surfaces for adenosine triphosphate (ATP), which is the energy molecule inside all living cells. ATP is found in bacteria, mold, fungus and other organic matter that can provide a rich food source for pathogens.
She listened attentively, occasionally nodding in agreement. Then she said something that I’ll never forget.
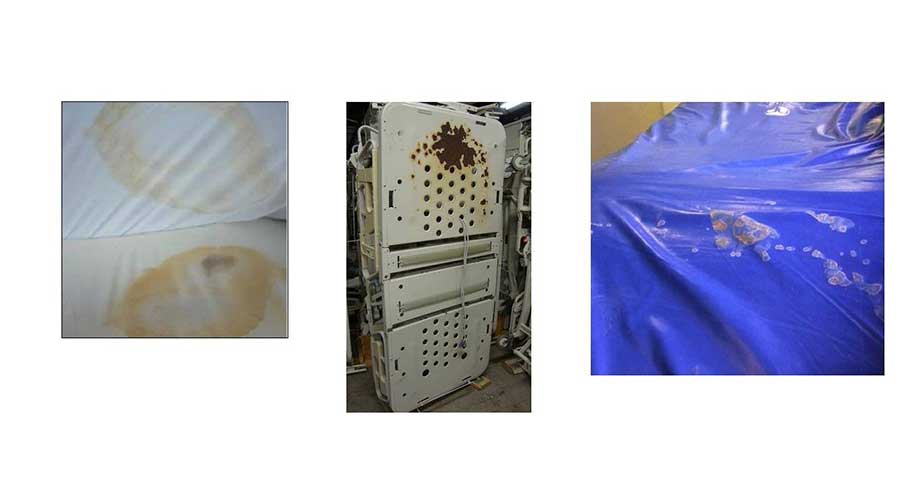
“Darrel, I appreciate the fact that we need to measure cleanliness to validate the work being done by the EVS tech assigned to that room. But I need to remind you that infection prevention is not always at the microbial level. When I can walk into a terminally clean room and find cookie crumbs between the bedrail and the frame, the bed isn’t ready for the next patient. Or when I can see red Jell-O on the surface of the children’s table in the corner of the room, I don’t need to qualify or measure the cleanliness of the room. It is obvious that we aren’t meeting a standard of care necessary for positive patient outcomes if the visible crud has not been removed.”
I didn’t get the job.
Unlike the COVID-19 virus, which spreads primarily through the air, bacterial and fungal organisms terrorizing hospitals are spread by touch and can last for weeks and months on surfaces. Masks are useless against most superbugs.
The stakes are too high to settle for the dirty status quo. A hospital patient who contracts a superbug faces a far higher risk of death than another patient with the same medical problem who does not get infected.
Infection prevention is not always at the microbial level.
The guiding principle is to always remove the obvious, visible soil. Washing or scrubbing a surface physically removes soil and organic material such as blood, Jell-O, cookie crumbs and body fluids.
J. Darrel Hicks, BA, MESRE, CHESP, Certificate of Mastery in Infection Prevention, is the past president of the Healthcare Surfaces Institute. Hicks is nationally recognized as a subject matter expert in infection prevention and control as it relates to cleaning. He is the owner and principal of Safe, Clean and Disinfected. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. He can be reached at darrel@darrelhicks.com, or learn more at www.darrelhicks.com.
 Design Plays a Role in the Future of Healthcare
Design Plays a Role in the Future of Healthcare Cedar Hill Regional Medical Center GW Health Officially Opens
Cedar Hill Regional Medical Center GW Health Officially Opens Designing Healthcare Facilities for Pediatric and Geriatric Populations
Designing Healthcare Facilities for Pediatric and Geriatric Populations Kaiser Permanente Announces New Hospital Tower at Sunnyside Medical Center
Kaiser Permanente Announces New Hospital Tower at Sunnyside Medical Center Building Disaster Resilience Through Collaboration
Building Disaster Resilience Through Collaboration