Patient safety is one of society’s greatest concerns. It might surprise some people, but attorneys play a major role in improving patient care. You might say they prefer clean hospital rooms over courtrooms. It also might surprise some to learn that no standards exist requiring a hospital room to be free of bacteria or viruses in sufficient numbers to cause an infection.
When a patient gets such an infection while receiving treatment for another condition, we call that a healthcare-acquired infection (HAI). These infections were not present when a patient was admitted to the hospital but developed in the hospital due to poor infection control.
As of 2011, there were an estimated 722,000 HAIs in U.S. acute care hospitals. Available evidence suggests this figure is down from 1.7 million in 2002. But HAI deaths are often misreported or underreported due to the potential for the assessment of Medicare penalties, according to Stanford University study.
The added financial burden attributable to HAIs is estimated to be $28-33 billion each year, according to the Agency for Healthcare Research and Quality. These are extremely high numbers, and they document a serious problem in our healthcare institutions.
Healthcare experts admit that HAIs have been a known problem for at least 40 years. Still, after substantial research and investment, the healthcare industry has not established a common and meaningful standard of cleanliness that patients can rely on.
Rather, healthcare facilities follow guidelines for cleaning rooms, and the guidelines have been known to be deficient for decades. A leading expert’s peer-reviewed conclusion was, “Unfortunately, environmental cleaning in healthcare facilities is often suboptimal.”
Related: The HAI That Never Happened
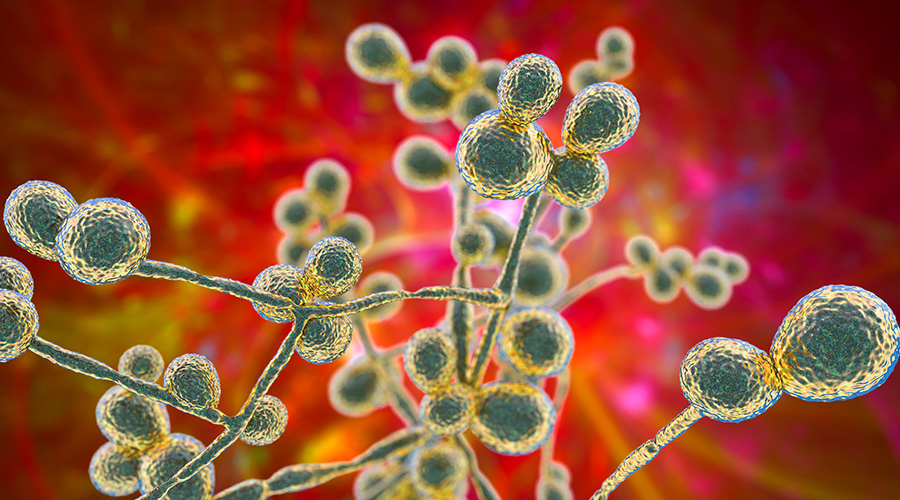
The most prevalent cleaning technique tasks a healthcare facility's non-medical staff with wiping high-touch surfaces using disinfectants, but this technique has been proven to leave more than 50 percent of the bugs — bacteria, as well as numerous viruses and spores — in place. Worse yet, studies have shown that some pathogens remain viable on hospital room surfaces for days and even months. Consequently, some healthcare institutions now combine standard cleaning practices with no-touch technologies.
Patients deserve better. One of the most widely accepted no-touch technologies, ultraviolet (UV) light has been shown to leave up to 35 percent of rooms with residual spores for Clostridium difficile, or C. diff, even when used in conjunction with bleach wipes.
We should work together to create a universal, meaningful standard of cleanliness. Hospitals can properly clean their rooms to make sure that the next patients put in them will not contract C-diff or other similar superbugs, but many still refuse to do so. Until all of them do, all we can do is ask if a patient's room was properly cleaned.
J. Darrel Hicks, BA, MESRE, CHESP, Certificate of Mastery in Infection Prevention, is the past president of the Healthcare Surfaces Institute. Hicks is nationally recognized as a subject matter expert in infection prevention and control as it relates to cleaning. He is the owner and principal of Safe, Clean and Disinfected. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. He can be reached at darrel@darrelhicks.com, or learn more at www.darrelhicks.com.

 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments