Making the invisible visible reveals opportunities for improvement, and that is exactly what an AirStatEQIairflow visualization technology can do for a healthcare environment. Because the SARS-CoV-2 is an enveloped RNA virus, it has the potential to exist in both droplet and aerosol forms and as a result can be transmitted very easily from person-to-person.
Furthermore, there is some evidence that this virus’ RNA can exist in an aerosol that could linger in the air, like the aerobiological properties of other viruses such as measles and Varicella zoster (chickenpox).
The Center for Disease Control (CDC) recommends that aerosol generating procedures (AGPs), such as intubation/extubation, or performing pulmonary procedures on COVID-positive patients should be performed in airborne infection isolation (AII) rooms (normally negatively pressurized).
Due to the surge in COVID 19 cases, the available AII rooms quickly reached capacity. As a result, some hospitals converted operating rooms (normally positively pressurized) or ICUs (with no air pressure requirement) to AII rooms under COVID surge conditions.
As new information is published on how the COVID 19 virus can spread, and as hospitals begin to reopen and perform non-emergent and elective surgeries, safety – of both patients and healthcare workers – will be paramount. Because spaces that were re-purposed during the pandemic will eventually be returned to their original intended function, the need for their environmental performance to be evaluated to ensure proper pressure, air flow patterns (clean to less clean), humidity, temperature, air change rates, and cleanliness (SARS-CoV-2 and mold free) will be required.
It is critically important to understand how the airflow can impact the time between scheduling procedures in different types of healthcare environments.
Validation that these recommissioned and reopened spaces are functioning optimally will play a big part in restoring consumer and employee confidence in healthcare providers and business owners. Accurate data and analysis can provide evidence that they have restored safe environments for their patients, visitors, and staff. The data and analysis can also serve for legal defense or protection from false claims.
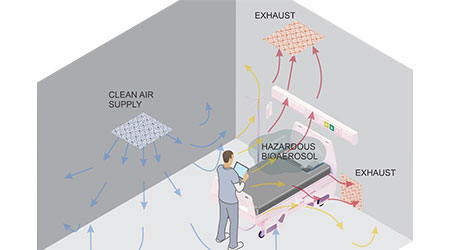
As a best-in-class practice, ventilation air movement should be from clean to less clean areas, while continuously exhausting potentially contaminated aerosols nearest to their source so that healthcare workers and uninfected patients in surrounding areas are protected from accidental exposure. This is achieved through directional flow of filtered supply air that carries infectious particles from their source to an exhaust inlet location.
Since air is invisible, a method is needed for visualizing how the directional air flows within the room. Because many spaces have been repurposed and are returning to their original use, it is important that this visualization is in real time or as frequently as possible. There are traditional methods, such as smoke tubes/generators that allow observation of the air direction; however, these can leave residues that can build up in a sterile environment. Hot wire anemometers are another airflow measurement technology in a specific location, but it does not measure air speed and direction, which is critically important to successfully operate safe healthcare environments.
This novel technology exists to empower safety, facility, or clinical rounding teams to ‘visualize’ airflow within a specific environment. The hand-held AirStatEQI Airflow Visualization Device measures and plots visually the velocity and directional flow of the air at various points within an AII room or procedural platform/OR space. Additionally, the instrument is highly accurate at extremely low air speeds down to 0.01 m/sec. By applying a proprietary risk mapping algorithm, the software can produce a ‘risk picture’ that instantly visually depicts how and where potentially contaminated air could harm healthcare works and/or escape into hallways and adjacent spaces. Please refer to Figure 1. If risks are identified, staff can then make alterations to work or patient care flows to mitigate any in-room risks.
The numerical risk readings are color coded green (in compliance), yellow (below target) and red (critical) on the picture for easy reference by the team member collecting the data. The risk readings can be uploaded to an interactive floor plan of the spaces (Figure 1), indicating location of key room furniture and fixtures in relation to the individual collecting the readings. In this figure, the AirStatEQI device is depicted in blue and its orientation is indicated for downdraft or cross draft readings at each specific location.
Depending on the complexity and layout of the room being measured, each reading location (2-10 per room) takes approximately 5 seconds (average 5 one-second readings) minimizing disruptions to patient care processes or procedures. Data from each reading is stored to enable analytics and trending of historical conditions.
Here are several examples of how hospitals have used this solution to reduce infection rates. A hospital in the Midwest recently used the patent pending algorithm, contained in the AirStatEQI Airflow Visualization solution, to predict risk of contamination by room sector. They substantially reduced their hospital acquired infections (HAI) in their OR suite. At another facility, this technology was used to identify the root cause of increased surgical site infections (SSI) to be airflow cross contamination. The Hospital made changes to the ventilation locations and rates, which resulted in a significant reduction in SSIs.
As mentioned above, at the start of the recent coronavirus pandemic, many hospitals were forced to repurpose spaces to be used as airborne infectious isolation rooms by reversing the directionality of the air to pull it through a high efficiency particulate filter and direct it out of the room. An unintentional consequence of this often placed the healthcare worker (HCW) between the patient generating the infectious aerosol and escape route of the, now contaminated, air. By visualizing the airflow patterns using the AirStatEQI, hospitals are empowered make informed decisions about how to reconfigure these spaces and where the HCWs are safest or at highest risk. This same concept has been used to better understand where HCWs should and should not reside in operating rooms during aerosol generating procedures. Often, HCWs not involved in the procedure would move the perimeter of the OR away from the patient in the sterile field. However, most of the time, the periphery of the OR is where the contaminants are at highest concentration by the nature of the downward flow of filtered air within the sterile field that is intended to wash the contaminants away from the patient and direct them out of the room through exhaust at the periphery.
By collecting data and reviewing regularly, the AirStatEQI Airflow Visualization Device allows hospitals to observe data patterns in real time that illustrate high risk areas that put patients and healthcare workers at risk. With a focus on risk prevention, identification and mitigation, the solution allows hospitals to take a proactive approach to harm reduction as it identifies risks and/or behaviors that can cause risk. This is especially important in today’s litigious environment.
Using the AirStatEQI Airflow Visualization Device regularly indicates that patient and healthcare staff safety is a top priority by providing legally defensible data regarding risk mitigation, which in turn will help restore patient and stakeholder confidence in healthcare organizations.
This novel technology exists to empower safety, facility, or clinical rounding teams to ‘visualize’ airflow within a specific environment.
Jennifer Wagner, Ph.D., CIC, is Managing Partner with Onsite, Northern CA. She can be reached at jwagner@onsite-llc.com. Ivan Maldonado is Founder and Managing Partner with Viu Insight Inc. He can be reached at ivan@viuinsight.com. Jeff Stephens is Managing Partner with Viu Insight Inc. He can be reached at jeff@viuinsight.com. Damon G. Greeley, PE, CEM, HFDP, CBCP, EDAC, CHFM, A-IPC, is Managing Partner with Onsite-LLC, Indianapolis, IN. He can be reached at dgreeley@onsite-llc.com.
 Healthcare Is the New Retail
Healthcare Is the New Retail Bridgeway Behavioral Health Services Launches Campaign to Renovate Health Center
Bridgeway Behavioral Health Services Launches Campaign to Renovate Health Center Ground Broken for New North Dakota State Hospital
Ground Broken for New North Dakota State Hospital AI Usage for Healthcare Facilities
AI Usage for Healthcare Facilities Ground Broken on Pelican Valley Senior Living Modernization Project
Ground Broken on Pelican Valley Senior Living Modernization Project