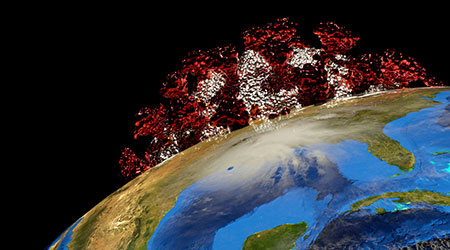
We are experiencing two crises at once: healthcare and hurricanes. How can our hospitals continue to fight on the frontlines of COVID-19 when one hurricane can upend everything?
As we know, the coronavirus has had a major impact on the healthcare delivery system across the country, with cases skyrocketing from single digits to millions in a matter of months. Hospitalizations have been steadily increasing as well, with the CDC forecasting 2,000-12,000 new hospitalizations per day. As if 2020 wasn’t busy enough, experts are now also labelling this year’s hurricane season as “extremely active,” with 18 named storms, “including 9 total hurricanes and 5 major hurricanes.”
It’s not luck that will keep our hospitals and other healthcare facilities in impacted areas functional, it’s preparation. Facilities must routinely research and update plans in order to reduce damage, remain open and recover quickly. Hospitals are a critical infrastructure asset for the community and need to provide care to those in need after a storm has passed, even as COVID-19 remains yet another storm to weather.
Here are four ways healthcare executives can prepare their facilities to withstand the shattering effects of both hurricane season and the global pandemic.
Plan and implement a comprehensive emergency management program
Healthcare facilities in the U.S. continuously fall short in disaster planning and preparedness. Having a well-established emergency management (EM) program lays the foundation for successfully addressing any unexpected crises. Planning for, responding to and recovering from a crisis is a multi-disciplinary effort, and an EM program’s and team’s strength is in the ability to help a facility through coordinating responses, planning through the disaster, and maintaining safety in times of uncertainty.
For hurricanes specifically, the detailed plan should cover monitoring, pre-landfall activities, equipment staging, risk assessments for wind or water damage, operations during the storm, and post-storm recovery. For the pandemic, consider including information on negative pressure rooms, controlling HVAC and other systems remotely, CDC guidance, supply chain management, signage and space reconfiguration, and more. Incorporating these details and prioritizing them based on the emergency or emergencies occurring will be crucial to reducing damage and costs while successfully maintaining operations.
EM also involves the expertise developed through planning and implementation, and the relationships built at the local, state, national and even global level. To create a successful program, it’s important to not just create one with the goal of meeting minimum regulatory requirements or saving money, but rather ensuring all facilities are prepared to serve their communities during great times of need.
Establish leadership and a diverse team of experts
One unforeseen hindrance many facilities run into with their EM program is leadership – or a lack thereof. Take your facility’s preparedness one step further by having the EM team designate an additional group of subject matter experts to tackle problems both within the facility and the multi-system organization as a whole. With this team, members can prepare guidance and navigate communication channels as they act as a liaison between the EM team, patients and staff. It’s important to gather top experts in a variety of fields – engineering, EM, operations, technology, construction, facilities management and more – to ensure all bases are covered.
Working in a variety of fields means the experts will be able to monitor facilities’ activity and adapt quickly to any situation in real-time during an emergency. This diverse team can collaborate and create solutions for what facilities need to do to adjust processes and programs to ensure safety. Maintaining this team even after the current emergency is crucial. Set up quarterly meetings with this group of experts to collaborate on and update existing plans, review new resources and inspire fresh ideas for the EM team.
In the case of a hurricane, leadership will play an integral role in decision making. Critical decisions such as additional resources and patient evacuation need to be made at least 48 hours before landfall, even as a storm’s impact area and intensity are unknown. The leadership team will also be responsible in determining staffing plans, canceling elective procedures, and closing off-site locations. Decisions should be coordinated with other hospitals in the impact area, as well. For example, if one hospital chooses to evacuate patients 48 hours ahead of landfall, while the other fails to evacuate and is unable to get out due to lack of resources or planning, that will greatly impact a community and its residents.
Determine the best channels for communication
Communication is essential for proper disaster preparedness. Whether communicating with staff, patients, government agencies or the public, healthcare facilities should establish these channels early. Staff communication in particular should be determined as part of the planning process to understand which staff may be available to assist during a disaster and any needs they may have, such as child or family care.
Patient and family communication is also critical, especially during COVID-19 when patients may be unable to receive in-person visitors. During a hurricane, for example, if patients’ families need to evacuate the area, the hospital’s ability to continue to communicate with them about the patient is vital. Patients, as well, should understand there is a plan to continue to provide care and keep them safe. If patients are evacuated, communicating with family members on where they are being moved and how to contact them is key.
Communicate early, often and accurately through regular updates, especially when there are a multitude of sources for the public to receive information. Social media, the internet in general and news channels (whether accurate or not) will all influence the public’s opinion. Control the conversation by utilizing a single expert source. Provide regular communication on facility response, updates on the outbreak or storm, and guidance to your facility teams. Focus on the information from the CDC as the source of truth, not cable TV or a tweet.
Evaluate and frequently update plans
Plans should be updated annually regardless. After an emergency, a thorough after-action review should be completed, including input from staff, patients and community response organizations. If any corrective actions are needed, a specific corrective plan should be written with leaders and timelines assigned. Once the corrective plan is completed, the updated plan should be tested through exercise, and staff should be reeducated on any changes to the plan.
As we’re currently in a predicted above-average hurricane season – in the midst of a global pandemic, no less – healthcare facilities are in a unique position to safeguard patients, staff and communities. How is your facility preparing to weather these two storms?
Scott Cormier is the Vice President of Emergency Management, Environment of Care (EOC) and Safety at Medxcel, ational network of hospitals that Medxcel serves.
 Severe Winter Weather: What Healthcare Facilities Must Prioritize
Severe Winter Weather: What Healthcare Facilities Must Prioritize Recovery Centers of America Opens New Facility in Florida
Recovery Centers of America Opens New Facility in Florida Munson Healthcare Caught Up in Third-Party Data Breach
Munson Healthcare Caught Up in Third-Party Data Breach From Downtime to Data: Rethinking Restroom Reliability in Healthcare
From Downtime to Data: Rethinking Restroom Reliability in Healthcare LeChase Building Four-Story Addition to UHS Delaware Valley Hospital
LeChase Building Four-Story Addition to UHS Delaware Valley Hospital