Candida auris (C. auris) is a type of fungus that can spread and prosper in healthcare settings. Disinfecting against it is a task in and of itself.
According to a study published in Clinical Infectious Diseases, researchers suspect that environmental contamination is a key factor in its transmission. After a room is disinfected, C. auris can quickly contaminate the healthcare environment again. This makes it challenging to keep the environment clean. The study suggests that future research should focus on finding disinfectants that last longer, surfaces that resist microbes, and better ways to clean patients' skin to reduce the presence of C. auris and other harmful bacteria in healthcare settings.
C. auris can be difficult for healthcare facilities to deal with and get rid of, as the Centers for Disease Control and Prevention (CDC) say that it not only leads to severe infections, but also lingers on surfaces for weeks and is hard to identify. Moreover, while the CDC says C. auris is a rare pathogen, they also report it has seen a 95 percent uptick in case rates from 2020 to 2021.
The rising incidence and newfound information shed light on the criticality of combatting C. auris effectively. To contain and fight the spread of this pathogen, HFT columnist J. Darrel Hicks recommends the following precautions:
- Make sure any hand sanitizers being used have a kill-claim listed for C. auris.
- Select a disinfectant from the Environmental Protection Agency’s (EPA) List K with the shortest and most realistic dwell time.
- Prior to using a List K disinfectant, check that it is compatible with the material of the patient care equipment.
- Isolated patients’ rooms must be processed twice daily by environmental services (EVS) in the day and night shifts. Any extra touches also need to be recorded as well.
- Have a defined process for notifying EVS leaders when cases of C. auris are isolated.
Jeff Wardon, Jr. is the assistant editor for the facilities market.
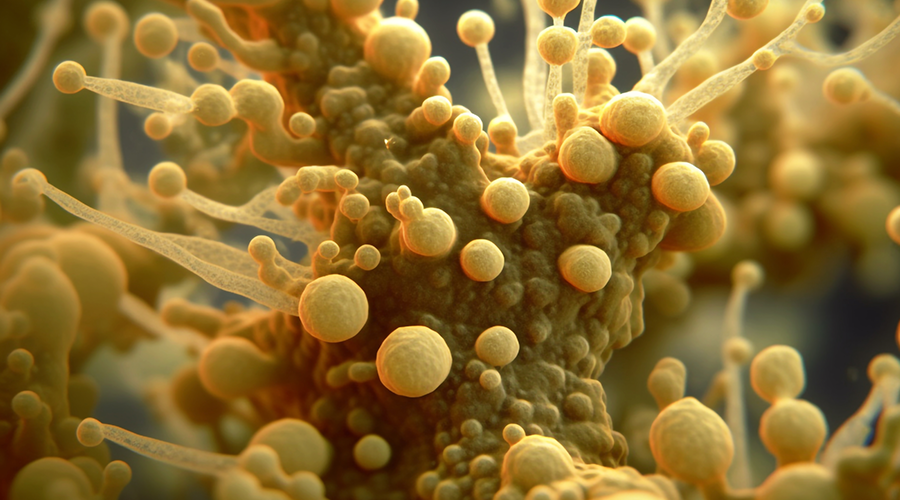
 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments