If one were to be admitted into a hospital patient room today and immediately noticed visible dust/dirt/blood on the medical equipment or obvious bodily fluid stains on the linens, they would be rightly horrified and disgusted. Thankfully, today’s healthcare facilities know and practice specific cleaning protocols to keep things clean and sanitary to prevent hospital-acquired infections (HAIs) and provide the best patient outcomes. In many cases, however, potential dangers are microscopic and hidden from the naked eye. Many of those microscopic dangers reside in dust, and when disturbed, they can travel throughout a healthcare facility undetected.
Dust consists of both live, dormant and decaying types of visible and microscopic particles. Some of these particles are essentially harmless (dust mites, dust mite feces, fibers) and some deadly (aspergillus, bacteria). A healthy person is often at a lower risk because the immune system is active and full-strength and can fight off those infections. In healthcare facilities, however, many patients have suppressed immune systems, and therefore the infection can spread rapidly with little or no response from the body’s immune system. In these types of cases, infected dust can be fatal. Protecting patients is a clear moral obligation.
While the moral obligation for hospitals to prevent HAIs is clear, there are also distinct business reasons that HAIs need to remain a priority for healthcare facilities. When a patient acquires an infection as a direct result of his or her hospital stay, the costs associated with that infection fall to the facility. Without insurance or Medicare reimbursement, HAIs can end up costing facilities thousands of dollars every year. It is in the best interest of both patients and facilities to minimize the possibility of healthcare acquired infections, and dust containment measures can help.
According to the Centers for Disease Control, 1 in 25 hospital patients in the U.S. have at least one hospital-acquired infection. In total, this means nearly 2 million infections each year and almost 100,000 deaths that can be traced back to HAIs. While HAIs have a range of contributing factors, proper dust containment procedures can be helpful in curbing the spread of disease. Pathogens from ceiling access maintenance as well as dust and debris that is roused during construction and renovations can be harmful to patients when inhaled. Further, contaminated dust can travel on staff and make its way into higher risk areas if it is not properly controlled.
The good news is that more and more hospitals are dramatically reducing this risk and offering assurances through the use proper dust containment measures, which means minimizing exposure to these particles through infection control protocols and the correct containment tools.
What is the art of containment?
While dust containment does have its critical share of calculations and measurements that are required to be effective, the truth is that there is both science and art that come into play. We define the art of containment with three simple rules:
• Choosing the best tools for the application
• Utilizing those tools in a competent way
• Looking 'good' doing it (where "good" means safe, serious and professional)
When a hospital or healthcare contractor can accomplish all three of the above, the result is a successful dust containment and infection control program that will dramatically reduce the risk of healthcare-acquired infections in patients and improve outcomes overall.
Influencing the art of containment are a variety of other factors including the evolving understanding of epidemiology, technology and patient care, legal and regulatory concerns, ROI, TCO, material costs, and the moral obligations of facilities to protect patients.
Choosing the best tools
The best tools for one containment project will not be the best tool for other instances, but there is certainly common ground to be found. Dust containment tools should be simple to use, easy to clean, and most importantly should be designed for maximum containment levels for the project. Containment standards any healthcare facility projects will depend on the ASHE Infection Control Risk Assessment Matrix and the Guidelines set forth by the Joint Commission.
A low-risk project will not need the same precautions that a high-risk task will need, so having tools and equipment that can handle a broad spectrum of applications is important.
Utilizing containment tools effectively
To use dust containment tools effectively, all staff using the tools must be properly trained in containment and the tools specifically. Though the best dust containment tools will be easy to use, it is important that staff know details like:
• When each tool is necessary for containment
• When a negative air machine with HEPA-filtration is necessary
• How to clean tools properly
• How many air changes per hour are required
• Where will the cleaned air be ported
Infection control personnel should have containment training programs in place, but it is the job of contractors to seek out the right training for themselves and their crew to ensure patient safety.
Looking good doing it
Patient safety is the goal of dust containment. However, patient safety and overall patient comfort depend on both the reality of the healthcare environment and the perception of that environment.
Protecting patients is serious business and by “looking good” while practicing the art of containment, we mean looking professional and proficient, in addition to creating an environment that in itself is good -- meaning it looks clean and safe. All professionals involved in dust containment procedures should maintain awareness of how they look as well as how their equipment looks.
The art of containment and healthcare acquired infections
Combining the art of dust containment with the science behind infection control, hospitals and contractors can continue to reduce the numbers of HAIs attributed to construction dust and continue to improve patient outcomes.
Mark Farnsworth is Vice President and General Manager at HEPACART, Inc.

 Reframing the Construction Manager as a Community Manager
Reframing the Construction Manager as a Community Manager Health First Celebrates 'Topping Off' Ceremony for New Cape Canaveral Hospital Campus
Health First Celebrates 'Topping Off' Ceremony for New Cape Canaveral Hospital Campus The University of Hawai'i Cancer Center Caught Up in Cyberattack
The University of Hawai'i Cancer Center Caught Up in Cyberattack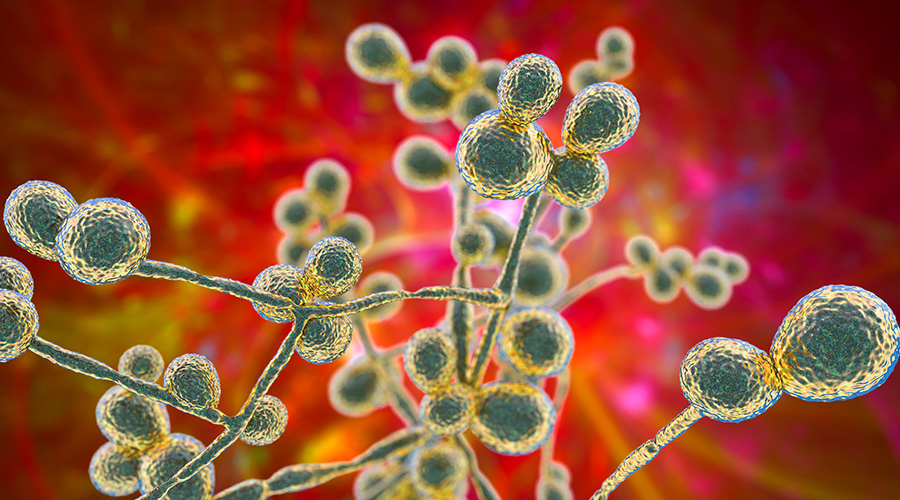 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens