How well do you know your enemy?
I recently participated in an outstanding webinar presented by Dr. Rodney Rohde, world-renowned microbiologist, regents' professor and global fellow at Texas State University. His co-presenter was Nicole Slacik, executive vice president healthcare with EvaClean Infection Prevention and Founder-Bextera Health. The webinar was entitled, “Candida auris and Biofilm: Proactive Measures for Mitigating Fungal MDROs.”
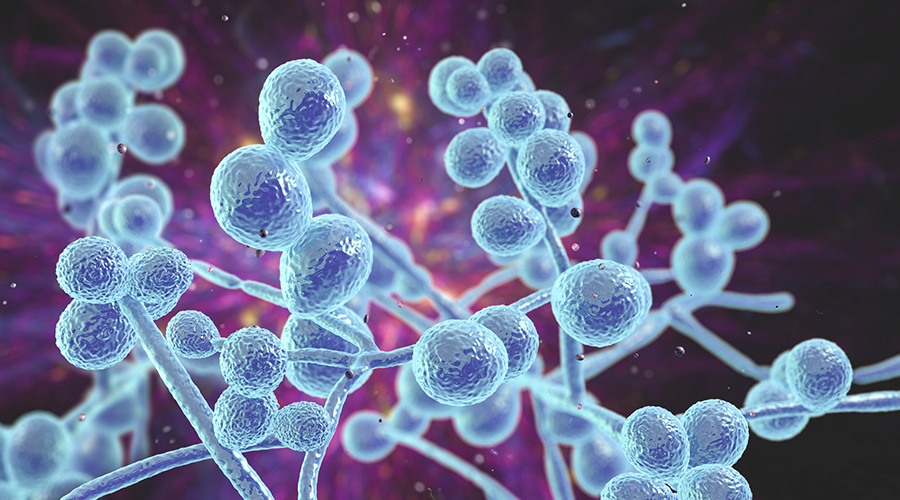
The webinar challenged attendees to “Know thy enemy,” as Sun Tzu said, and to prepare for the war with Candida auris (C. auris) and especially biofilm. As a veteran of the war against healthcare-acquired infections, I became keenly aware of the way this enemy can create an Iron Man-like suit of armor called biofilm.
The C. auris fungus can survive for weeks on surfaces in hospitals and other healthcare facilities. An environmental reservoir such as a biofilm tends to enable its persistence and ability to survive on surfaces and devices even longer, even up to months. When C. auris becomes firmly entrenched on patient care equipment and environmental surfaces, it is nearly impossible to eradicate without a hospital-wide, sporicidal disinfectant with a kill-claim for C. auris and biofilm.
This disinfectant should appear on U.S. Environmental Protection Agency (EPA) P and K lists to disinfect computers on wheels, mobile radiology equipment, glucose meters, walkers, wheelchairs, stretchers, patient lifting equipment and other items rolling in and out of patient rooms. The nursing station, staff breakroom, pantry and other middle areas of patient care divisions should be included in targeted disinfection at least once daily.
The EPA letter list tests are for isolate/planktonic cells in suspension to make kill claims on a claim on an EPA letter list, not cells taken from the natural environment that may be found in a protective layer of bacterial biofilm. That is why environmental services (EVS) managers should not rely upon only current EPA letter lists when evaluating disinfectants. C. auris is well known to thrive in biofilm.
Many common disinfectants do not have the ability to kill bacteria in biofilm, but there is an EPA test for a disinfectant biofilm claim. This claim can be found on a product’s master label by using the EPA registration number on the product’s label.
Consider this proactive protocol for isolation rooms: Although C. auris contaminated surfaces — think high-touch surfaces — are disinfected to a fit-for-purpose level during the daily patient room processing by the EVS technician, those surfaces should be re-processed a second time by EVS. Studies have proven that high-touch contamination rebounds within four to six hours, post processing.
The term process includes cleaning and disinfecting a piece of patient care equipment or a patient care area using micro-denier cloth or flat mop, as appropriate, and a hospital-approved disinfectant. Workers don’t clean a patient’s room. They process it. They don’t clean an operating room. They process it.
One EVS technician educated about the way C. auris spreads in the environment, given the right disinfectant and the proper amount of time to do the task, can prevent more C. auris than a roomful of doctors can cure.
J. Darrel Hicks, BA, MESRE, CHESP, Certificate of Mastery in Infection Prevention, is the past president of the Healthcare Surfaces Institute. Hicks is nationally recognized as a subject matter expert in infection prevention and control as it relates to cleaning. He is the owner and principal of Safe, Clean and Disinfected. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. He can be reached at darrel@darrelhicks.com, or learn more at www.darrelhicks.com.
 UF Health Hospitals Rely on Green Globes to Realize Their Full Potential
UF Health Hospitals Rely on Green Globes to Realize Their Full Potential How Healthcare Facilities Can Be Truly Disaster-Resilient
How Healthcare Facilities Can Be Truly Disaster-Resilient TriasMD Breaks Ground on DISC Surgery Center for San Fernando Valley
TriasMD Breaks Ground on DISC Surgery Center for San Fernando Valley Bigfork Valley Hospital Falls Victim to Data Breach
Bigfork Valley Hospital Falls Victim to Data Breach AI-Driven Facilities: Strategic Planning and Cost Management
AI-Driven Facilities: Strategic Planning and Cost Management